RHEUMATIC DISEASES AND THE EYE CARE AND PROBLEMS IN RA PATIENTS

Dr Udayan Dixit
Consultant Ophthalmologist
dudayan@hotmail.com
98220 57734.
Aches and pains, limitations in movements , prolonged and relentless course of the disease and restrictions in so many day to day activities is how everyone knows the Rheumatic Diseases [RD]. Mostly seen in adults and the elderly but this enigma of a disorder unfortunately can affect even young children although thankfully on relatively lesser occasions .
Affection of the eye and that too sometimes with grave possible consequences is not something which the patients of RD are aware of . Conditions like Rheumatoid Arthritis, Systemic Lupus Erythematosus, Psoriatic Arthritis, Juvenile Idiopathic Arthritis [JIA] , Juvenile Seropositive Arthritis , Ankylosing Spondylitis are some of the Rheumatic Diseases which affect the eyes.
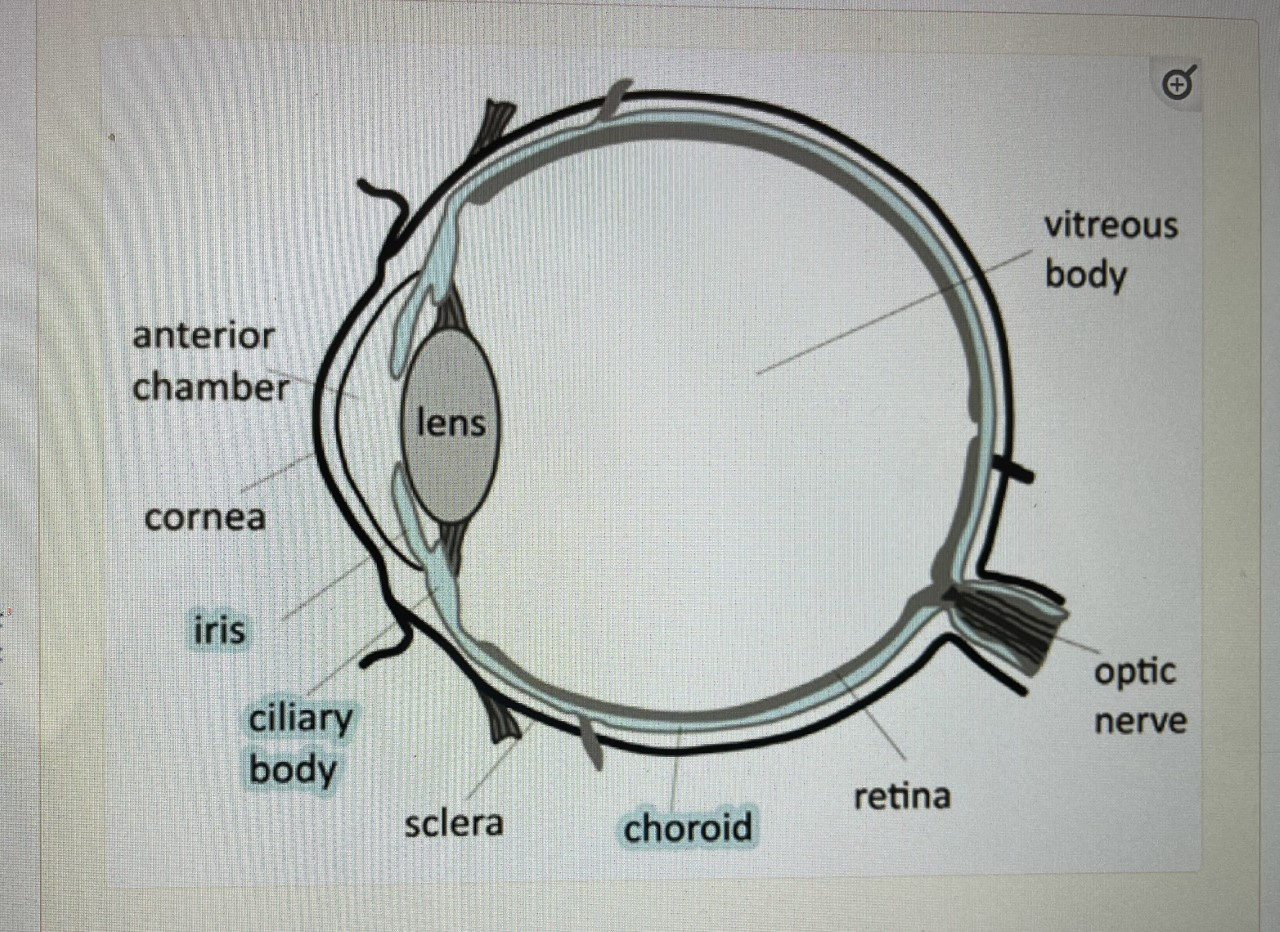
Many parts of the eye can be affected by RD . In fact sometimes the eye is an important indicator of the onset and progression of the disease . It is not necessary that an attack of Arthritis will match an attack of an Inflammatory Episode of the eye . From the front or the anterior segment to the backmost part of the eye or posterior segment , all the layers can get affected by RD.
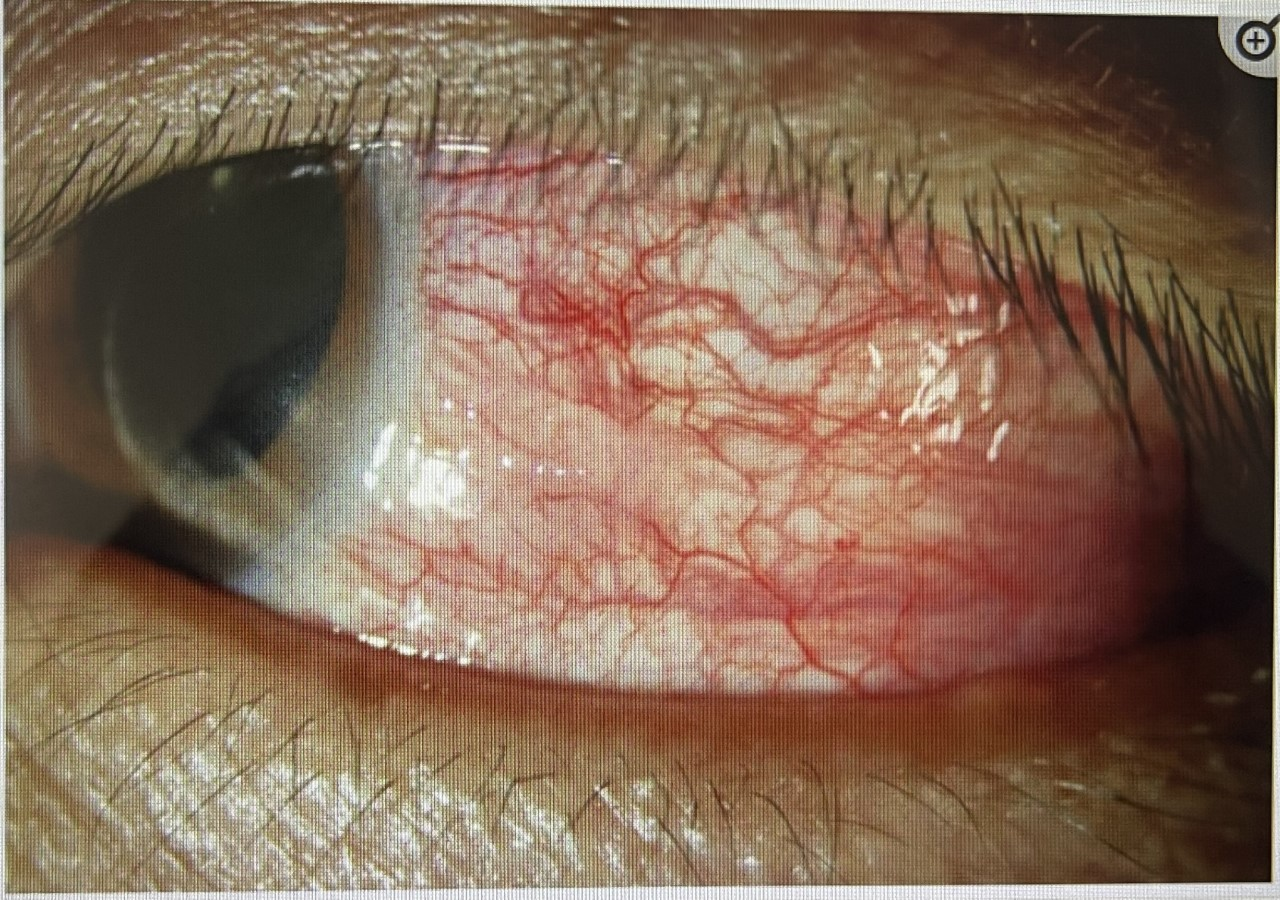
1] A patient starts complaining of pain, redness, watering , mild reduction in vision ,sensitivity to bright light These are the symptoms of the commonest disorder of the eye related to RD . It is called Iritis or Iridocyclitis.
The more precise name for the same is “ Acute Anterior Uveitis” . It is important for the eye doctor to have high index of suspicion in patients presenting with these symptoms , specially in case of someone with a known history of RD .A simple but careful clinical examination on the Slit Lamp Bio Microscope can clinch the diagnosis
The doctor can see presence of cells and fogginess in the front compartment of the eye called “ Anterior Chamber”.
The treatment has to commence immediately . It is usually in the form of eye drops . Anterior Uveitis can occur repeatedly . Each episode can leave behind a legacy like adhesions between the pupil and anterior lens capsule called “Anterior Synechiae.”
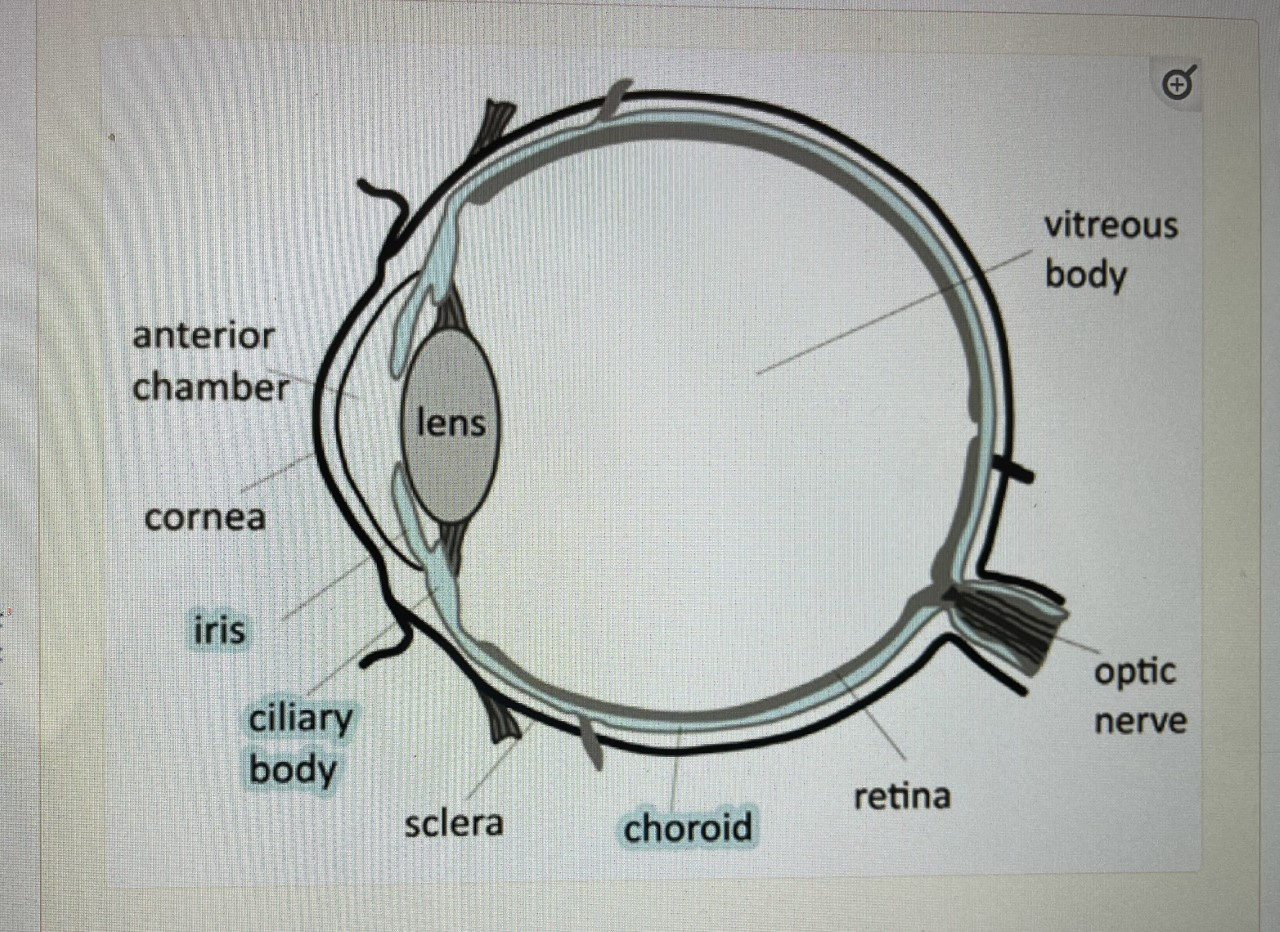
Schematic diagram of the eye.
Local steroid drops and pupil dilating or mydriatic drops is the mainstay of treatment for Iritis and Iridocyclitis [ Acute Anterior Uveitis ] .On occasions , patient who show a serological test called HLA B27 positive , the course of anterior Uveitis is more severe . A pus like level is seen in the area between cornea and iris . This is called Hypopyon . This requires intense local medication and help of oral medication may be required . In children Anterior Uveitis is noted in cases of Juvenile Idiopathic Arthritis [ JIA] . In these patients , the eye can be quiet unlike adult Acute Anterior Uveitis and hence a diagnosis can be missed unless one is vigilant during eye examination.

Pupil adhesions or Synechiae.

Hypopyon
On rare occasions , when Anterior Uveitis is non responsive to steroid regimen , immunosuppressants like Methotrexate, Azathioprine on TNF inhibitors like Infliximab or Adalimumab are used .
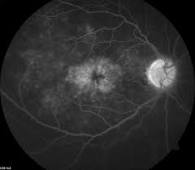
2] Sometimes the back portion of the eye called posterior segment gets affected by a few varieties of Rhematic Diseases . This disorder is called Choroiditis wherein the layer behind the retina gets inflamed . Retina itself can get affected too when it is called Retinitis . Patients with posterior segment disease can complain of Floating particles in front of the eye and reduction of vision . Diagnosis is made by careful examination of the back of the eye called Fundoscopy examination . Ancillary tests like Photography of the back portion of the eye after injecting a dye into the vein of the hand ,called Fundus Fluorescein Angiography [ FFA] ,ICG dye Angiography and retinal scan called OCT are done.
In some patients , the anterior , intermediate and posterior segment of the eye, all get inflamed . This condition is called “ Pan uveitis”.
The posterior segment inflammations require oral medication . It is in the form of anti inflammatory drugs , mainly oral steroids . On some occasions the disease does not come under control with steroids or keeps relapsing as soon as the dose of steroids is lowered to safe levels . I this situation , drugs called Immunosuppressants or anti metabolites are used . Cyclosporine, Tacrolimus, Mycophenolate Mofetil, Rituximab are some of the drugs used for severe posterior uveitis . Modern drugs called Biologics are now used more effectively for the posterior segment affection of the eye caused by RD . Long term steroid treatment has to be carefully monitored . Weight gain, puffiness of face , rise of blood sugar and blood pressure , acidity or gastritis, bone density lowering or Osteoporosis are known untoward effects of long term oral steroids . If one considers treatment with Antimetabolites or Biologics , it is advisable for eye doctors to work as a team with Rheumatologists. These new drugs can have detrimental effects on Kidney , Liver and immunity of the patients.
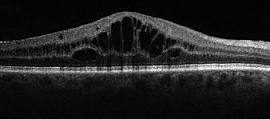
3] On occasions the central part of retina called as Macula gets swollen [ Macular Edema ] in patients with RD . . This is commonly seen in “ Intermediate Uveitis” where the part between anterior and posterior segment of the eyeball called Pars Plana gets inflammation . Macular Edema causes rapid reduction of central vision . Diagnosis can be made by simple clinical examination with special lenses in front of the Slit Lamp Biomicroscope . Confirmation and grading of Macular Edema is done by doing Retinal Scan called OCT [ Optical Coherence Tomography ] . The most effective treatment of Macular Edema is in the form of injection of steroid given in the jelly that is present in front of retina called “ Vitreous Humor”. This intra vitreal injection is given under topical anesthesia or by instillation of eye drops , under the microscope and takes only two minutes to administer it .