Rheumatic Disorders of neck & back – Signs,symptoms & diagnosis

Dr.Rahul Patil
Neck & back pain is one of the most common complaints seen in the clinics/hospitals. It is reported that at least 80% of the general population will at one time or another during their lifetime experience significant back pain. The vast majority of these back pain episodes are related to muscle spasm or degenerative joint and disc disease of the lumbar spine or sacroiliac joints. Typically these “mechanical” back pain problems can be attributed to trauma and usually get better with rest and are worsened by activity. A much smaller percentage of patients, perhaps 0.5% – 1.0% of the population will experience “atypical” back symptoms which suggest “inflammatory back pain” which are due to rheumatic diseases. The hallmarks of inflammatoryback pain that distinguish it from the more common types of mechanical back pain include:
1.Onset typically in young adults
2.Insidious onset without specific inciting event
3.Present for greater than 3 months
4. Prolonged morning stiffness
5.Improves with activity

These rheumatic diseases of neck & back can be classified as:
•Inflammatory
o SeronegativeSpondyloarthropathies (SSA)
o Rheumatoid Arthritis (RA)
o Polymyalgia Rheumatica
•Mechanical
o Osteoarthritis
•Miscellaneous
Seronegative Spondyloarthropathies
The prototypic inflammatory back disease is Ankylosing Spondylitis, although there are several associated disorders which share similar features and are collectively known as “seronegativespondyloarthropathies.” The associated disorders include Psoriatic spondyloarthropathy (associated with psoriasis), Reactive arthritis (seen following infections of the gastrointestinal or genitourinary systems), as well as inflammatory bowel diseases such as Ulcerative Colitis and Crohn’s disease.
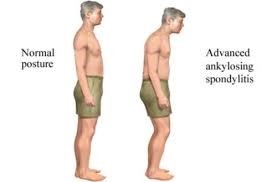
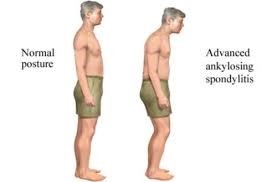
Fig:1 Posture of patient with SSA.
In addition to sharing inflammatory back pain symptoms, these disorders collectively share other features that differentiate them from mechanical back pain. These shared features include:
1. Predilection for young adults with increased severity in males
2. Familial aggregation due to association with a genetic marker known as HLA-B27.
3. Negative blood work for rheumatoid factor and other auto antibodies
4. Predilection for the sacroiliac joints and spine
5. When peripheral joints are involved, it is often the large joints of the lower extremities in an asymmetric pattern (both sides of the body are not equally affected)
6. Tends to involve the enthesis (area of ligament and tendon insertion into bones) resulting in heel and Achilles tendon pain, as well as dactylitis (sausage like swelling of the digits) which is a diffuse swelling of fingers and toes.
7. Involvement of extra-articular organ systems including:
a. Eyes – episcleritis, scleritis, iritis
b. Skin – psoriasis and psoriasis-like rashes
c. Mucous membranes – ulcerations
d. Lung – pulmonary fibrosis
e. Cardiac – aortic insufficiency and cardiac conduction disturbances
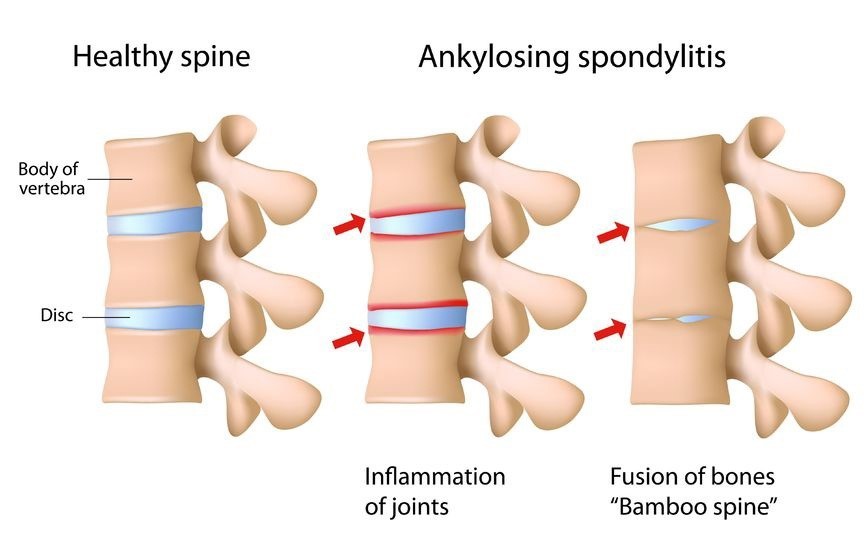
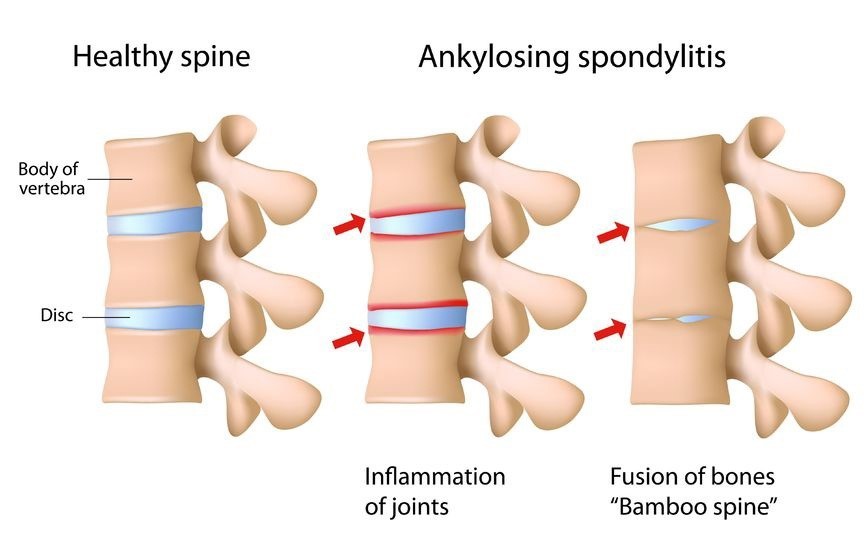
Fig:2 Pathological changes at spinal level in patients with SSA.
Diagnosis:
Laboratory studies provide very little help in making a diagnosis, although one may have a mild anemia and have an elevated sedimentation rate consistent with inflammation. Occasionally, obtaining the genetic marker HLA-B 27, can assist in making a diagnosis in difficult situations. X-rays are often very helpful, with abnormalities identified in the sacroiliac joints and lumbar spine, however these typically appear late, often after 10 years of disease duration. MRI studies are often able to identify the inflammatory changes in the sacroiliac joints much earlier in the disease course allowing for an earlier diagnosis and treatment intervention.
Rheumatoid Arthritis in the neck
Rheumatoid arthritis (RA) is a chronic inflammatory disease where the body’s immune system mistakenly attacks the lining of the joints. An overactive immune system causes an inflammatory response, resulting in symptoms, such as pain, swelling, and stiffness.
Rheumatoid arthritis can start in the smaller joints of your hands and feet. As the disease progresses, however, it can spread to other parts of your body like the neck. This doesn’t typically happen until years after the onset of arthritis symptoms.

Fig:3 Pathological changes in the cervical spine in patients of RA in the neck.
Chronic inflammation in the neck causes the destruction of the synovial joints, which are the joints that allow movement. When arthritis damages this joint in the neck, the cervical spine can become unstable.
Vertebrae are small bones that form the backbone. There are seven, and rheumatoid arthritis typically affects the first and second, called the atlas and axis, respectively.
The atlas supports the weight of your head and the axis helps your neck move in different directions.
An unstable vertebra can shift or dislocate over time and eventually press on the spinal cord and nerve roots. When this happens, you may have numbness and tingling around the neck that radiates up the back of the head. This is in addition to joint pain, stiffness, and swelling.
Diagnosis:
A physical exam can help gauge the range of motion in your neck, and it can reveal signs of joint instability, inflammation and misalignment.
There isn’t a single test to diagnose RA, but you may be asked for a series of tests to reach this conclusion.
This includes blood work to look for inflammatory markers and auto-antibodies that are often indicative of RA.
You may also undergo an imaging test which takes picture of the inside of your body, such as an X-ray, MRI, or an ultrasound.
These tests are helpful for determining the extent of inflammation and joint damage in the neck.
Polymyalgia rheumatica
Polymyalgia rheumatica is an inflammatory disorder that causes muscle pain and stiffness in various parts of the body. It most commonly affects the:
• shoulders
• neck
• arms
• hips
The symptoms often appear suddenly and tend to be worse in the morning. Polymyalgia rheumatica typically affects people over age 65. It rarely develops in those under age 50. Polymyalgia rheumatica is also more likely to occur in women than in men.
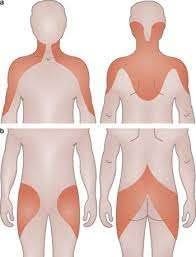
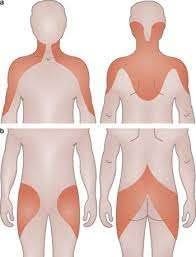
Fig:4 Areas of pain & tenderness in patients of Polymyalgia Rheumatica.
Pain and stiffness in the neck and shoulders are the most common symptoms of polymyalgia rheumatica. The pain and stiffness may gradually spread to other areas, such as the shoulders, hips, and thighs. These symptoms usually affect both sides of the body.
Other common symptoms of polymyalgia rheumatica include:
• fatigue
• malaise
• a loss of appetite
• sudden, unintentional weight loss
• anemia, or low red blood cell count
• depression
• a low-grade fever
• a limited range of motion
Diagnosis:
The symptoms of polymyalgia rheumatica can be similar to those of other inflammatory conditions, including lupus and arthritis. To make an accurate diagnosis, you may undergo physical examination and run several tests to check for inflammation and blood abnormalities.
If polymyalgia rheumatica is suspected, they may order blood tests to check for signs of inflammation in your body. These tests will measure your erythrocyte sedimentation rate and C-reactive protein levels.
You may also need an X-ray, an ultrasound or MRI to check for inflammation in your joints and tissues.
Osteoarthritis spine
Osteoarthritis (OA) is a degenerative joint disease. This disease is caused by the deterioration of cartilage. This is the smooth, elastic tissue that protects joints and provides the lubrication necessary for normal jointfunction.
Osteoarthritis can affect different joints in the body, such as those in the:
• hands
• knees
• hips
• spine
OA of the spine specifically affects the facet joints, the cartilage between the bones that make up the spine, and the ligaments in the spine.
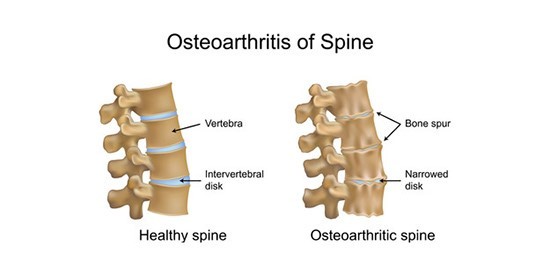
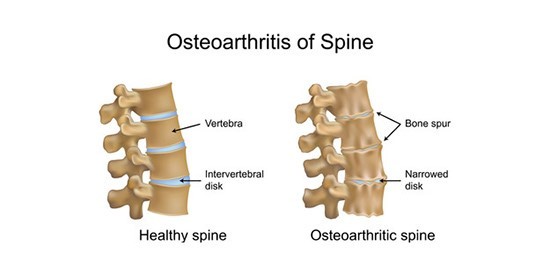
Fig:5 Pathological changes in the spine in patients with OA spine.
As you age, the cartilage coating the facet joints can slowly wear away. Your invertebral discs are made primarily of water. These discs can dehydrate as you grow older. This can cause the discs in your spine to narrow and put increased pressure on facet joints.
OA of the spine causes various symptoms. The most common is back pain. Pain often starts in the lower back. In the early stages of the disease, you may only have pain in the mornings due to hours of inactivity. Since this is a progressive disease, symptoms typically worsen over time. Other symptoms of osteoarthritis of the spine include:
• joint tenderness
• joint stiffness
• limited range of motion
• weakness or numbness in the legs or arms, tingling in the legs
Back pain caused by OA of the spine is often worse when sitting upright or standing. It usually improves when lying down. Some people who have osteoarthritis of the spine don’t have any symptoms.
Diagnosis:
Before diagnosing OA of the spine, you may be asked about your family history of the disease and a complete physical examination to check for tenderness, limited range of motion and swelling in your back.
Imaging tests are commonly used to diagnose OA of the spine. These tests can check for bone damage, bone spurs, and loss of cartilage in your joints. You may be asked for an X-ray or an MRI, which creates a detailed picture of your spine.
Sometimes joint fluid analysis may be done. In this procedure, your doctor inserts a needle in the affected joint to collect a fluid sample. This test can determine whether symptoms are caused by OA, gout, or an infection.
Miscellaneous causes of low back pain include:
• Fibromyalgia
• Functional Disorders
• Osteoporosis