LOW BACK PAIN (LBP)
by Dr KIRAN ADAM
Low back pain(LBP) is not a specific disease but rather a complaint that may be caused by a large number of underlying problems of varying levels of seriousness. The majority of LBP does not have a clear cause but is believed to be the result of non-serious muscle or skeletal issues such as sprains or strains.Obesity, smoking, weight gain during pregnancy, stress, poor physical condition, poor posture and poor sleeping position may also contribute to low back pain A full list of possible causes includes many less common conditions. Physical causes may include osteoarthritis, degeneration of the discs between the vertebrae or a spinal disc herniation, broken vertebra (such as from osteoporosis) or, rarely, an infection or tumor of the spine.
Low back pain(LBP) can be broadly classified into four main categories:
- Musculoskeletal - mechanical (including muscle strain, muscle spasm, or osteoarthritis); herniated nucleus pulposus, herniated disk; spinal stenosis; or compression fracture,
- Inflammatory - HLA-B27 associated arthritis including ankylosing spondylitis, reactive arthritis, psoriatic arthritis, and inflammatory bowel disease
- Malignancy - bone metastasis from lung, breast, prostate, thyroid, among others
- Infectious - osteomyelitis; abscess
In this article will be focusing on Ankylosing Spondylitis(AS)
Ankylosing Spondylitis(AS)
The word is from Greek ankylos meaning stiffening, spondylos meaning vertebra, and a it is meaning inflammation.
What is Ankylosing Spondylitis(AS) ?
Introduction-Ankylosing spondylitis is classified along with the seronegative spondyloarthritic diseases. Ankylosing spondylitis is a chronic, systemic, inflammatory disease that affects primarily the sacroiliac joints and spine. Certain peripheral joints and tendons can also be affected, and extra-articular manifestations may be present. The disease typically affects young adults, and there are strong genetic features.
Prevalence of AS is 0.1 % to 1.4 % depending on population studied AS is predominanty seen in young Men,Women also suffer though infrequently.
What causes Ankylosing Spondylitis?
The etiology of ankylosing spondylitis remains unclear. There is solid evidence pointing to a genetic component and risk. The HLA B27(Human leucocyte anigen) gene is commonly present, and there is a strong familial association. Infective mechanisms have been proposed but seem less evident than in the reactive arthritides. The spondyloarthritides, as a subset, have several distinguishing features that are shared among them. The diseases are seronegative by definition. There are common genetic factors including the human leukocyte antigen (HLA) B27 gene. Axial involvement, including sacroiliitis, can be seen in all and is essential for the diagnosis of ankylosing spondylitis. Enthesitis, or inflammatory changes of the tendon and ligament attachment to bone, is the primary pathologic phenomenon. The spondyloarthritides share many extra-articular features including uveitis, psoriasis and colitis.
What are signs & symtoms of Ankylosing spondylitis?
AS is much more common in young men. Onset before age of 40 years. Initialsymtoms are usually a chronic dull pain in lower back more than 3 months duration Early morning stiffness > 30 Min. Alternate buttock pain with stiffness of LBP. Individuals often experience pain & stiffness that awakens them in the early morning. AS can occur in any part of spine or entire spine often with pain reffered to one or other buttock or back of the thigh from sacroititis. Asymmetrical Arthritis predominantly lower limbs (knees,ankle) Immprovement of symtoms with exercise,but not with rest. pain and swelling may also manifest in the ankles and feet where heel pain and enthesopathy commonly develop. Sausage of fingers or toes(dactylitis) About 40% of people with AS will also experience inflammation of the anterior chamber of the eye, causing eye pain, redness, floaters and sensitivity to light(Uveitis). Signficant family history ( AS, Psoriais , inflammatory bowel diseases(IBD),HLA B27 ).
How is Ankylosing SpondylitisDignosed
Inflammatory back pain:
- Chronic, inflammatory back pain is defined when at least four out of five of the following parameters are present:
- (1) Age of onset below 40 years old, (2) insidious onset, (3) improvement with exercise, (4) no improvement with rest, and (5) pain at night (with improvement upon getting up)
- Past history of inflammation in the joints, heels, or tendon-bone attachments.
- Family history for axial spondyloarthritis.
- Positive for the biomarker HLA-B27.
- Good response to treatment with nonsteroidal anti-inflammatory drugs (NSAIDs).
- Signs of elevated inflammation (C-reactive protein and erythrocyte sedimentation rate).
- Manifestation of psoriasis, inflammatory bowel disease, or inflammation of the eye (uveitis).
Radiographic features
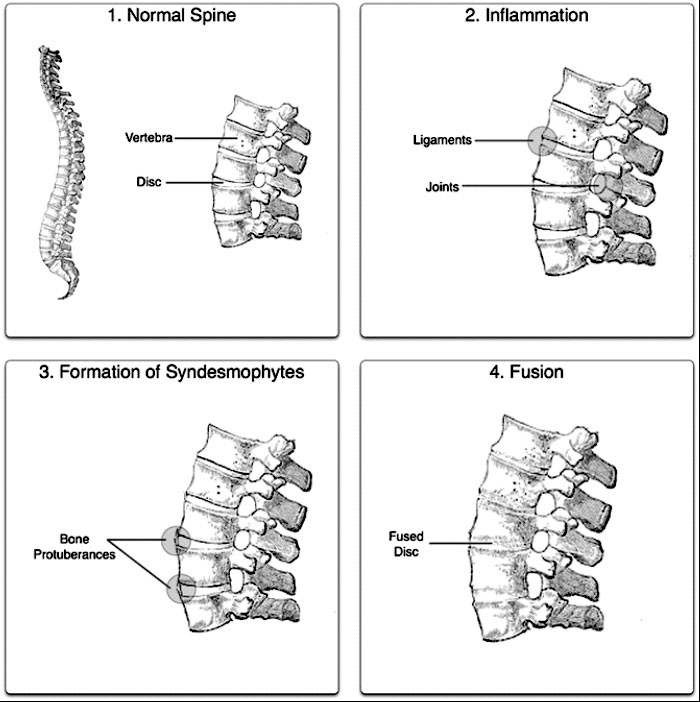
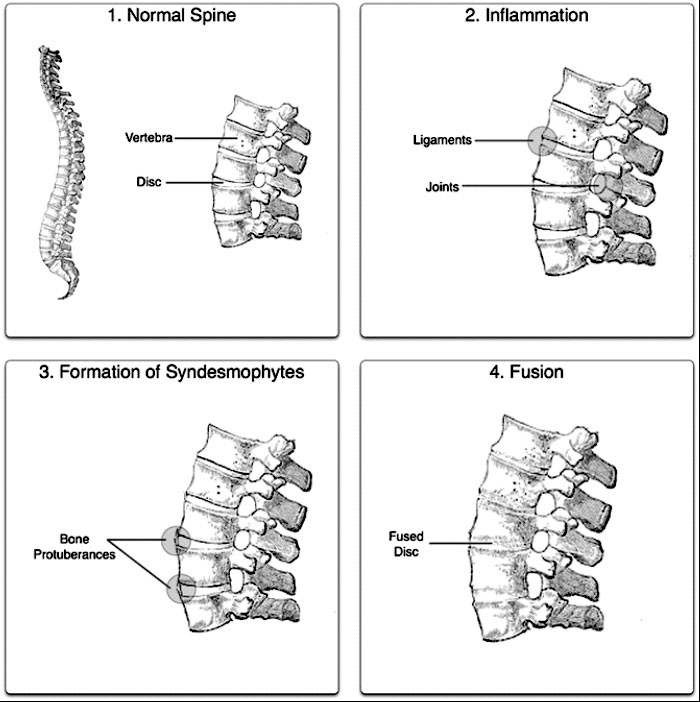
- The earliest changes in the sacroiliac joints demonstrable by plain x-ray shows, sacroilitis, erosions and sclerosis.
- Progression of the erosions leads to pseudowidening of the joint space and bony ankylosis.
- Positive for the biomarker HLA-B27.
- X-ray spine can reveal squaring of vertebrae with spine ossification with fibrous band run longitudinally called syndesmophyte while producing bamboo spine appearance.
- A drawback of X-ray diagnosis is the signs and symptoms of AS have usually been established as long as 10 years prior to X-ray-evident changes occurring on a plain film X-ray, which means a delay of as long as 10 years before adequate therapies can be introduced. Options for earlier diagnosis are tomography and MRI of the sacroiliac joints.
How is Ankylosing Spondylitis treated?
The major types of medications used to treat ankylosing spondylitis are pain-relievers and drugs aimed at stopping or slowing the progression of the disease. All of these have potentially serious side effects. Pain-relieving drugs come in two major classes:
- The mainstay of therapy in all seronegative spondyloarthropathies are anti-inflammatory drugs, which include NSAIDs such as ibuprofen, diclofenac, indomethacin, naproxen and COX-2 inhibitors( etoricoxib), which reduce inflammation and pain. Indomethacin is a drug of choice. 2012 research showed that those with AS and elevated levels of acute phase reactants seem to benefit most from continuous treatment with NSAIDs.
- NSAIDS are safe when used with care.but they have several side effects when used in high, unregulatedquantities, unsupervised & for prolonged periods.
Medications used to treat the progression of the disease include the following:
- Disease-modifying antirheumatic drugs (DMARDs) such as sulfasalazine can be used in people with peripheral arthritis. For axial involvement, evidence does not support sulfasalazine. Other DMARDS, such as methotrexate, did not have enough evidence to prove their effect. Generally, systemic corticosteroids were not used due to lack of evidence. Local injection with corticosteroid can be used for certain people with peripheral arthritis.
- Biologic Drugs-these are antibodies which attacks the immune cells or their products (like cytokines) thus biologic drugs can stop the initial disease process event and cause early improvement & arrest the disease process,which includes,Tumor necrosis factor - alpha (TNFÎą) blockers (antagonists), such as the Biologics Etanercept, Infliximab, Golimumab and Adalimumab, have shown good short-term effectiveness in the form of profound and sustained reduction in all clinical and laboratory measures of disease activity .
- Only Rheumatoligst are authorized to use biologics DMARDS .these drugs are often given into blood circulation (intravenously) and require close monitoring of blood pressure and any allergy response.special infusion pumps are often required to monitor the rate of the drug when given intravenously.
- Besides drugs ,there are several other important treatment modalities, Physiotherapy,swimming including exercises can improve measures of pain , spinalmodalities, patientfunctioning, maintain posture & well- being.
- Some modifications in the life style such as smoking has been associated with a poor functional out come& encouraged to quit.